Nclex questions acute kidney injury – Embark on a journey into the realm of NCLE questions on acute kidney injury. This comprehensive guide will illuminate the complexities of this condition, empowering nurses with the knowledge to confidently navigate the challenges it presents.
Acute kidney injury, a prevalent concern in healthcare, demands a thorough understanding of its pathophysiology, clinical manifestations, and nursing management strategies. This guide delves into the intricacies of the condition, providing nurses with the essential tools to excel in patient care.
Understanding Acute Kidney Injury: Nclex Questions Acute Kidney Injury
Acute kidney injury (AKI), formerly known as acute renal failure, is a sudden loss of kidney function. It can range from mild to severe and can be caused by a variety of factors, including dehydration, sepsis, and certain medications. AKI can lead to a buildup of waste products in the blood, which can be life-threatening if not treated promptly.
Pathophysiology of Acute Kidney Injury
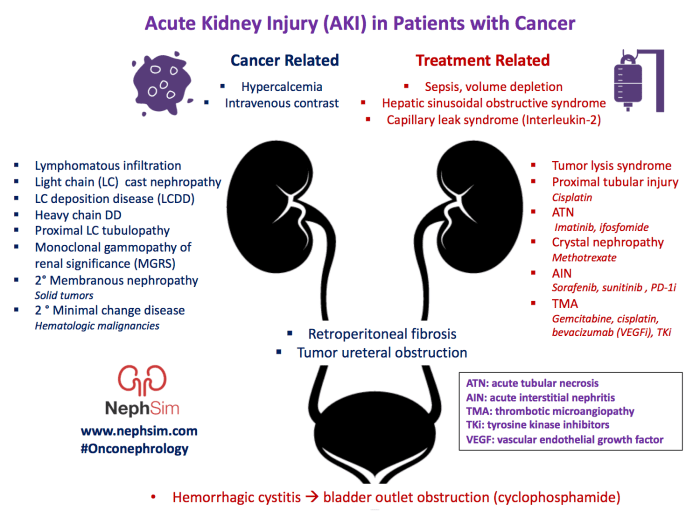
The pathophysiology of AKI is complex and involves a number of different mechanisms. In general, AKI occurs when the kidneys are unable to filter waste products from the blood. This can be caused by a decrease in blood flow to the kidneys, damage to the kidney cells, or obstruction of the urinary tract.
- Decreased blood flow to the kidneyscan occur due to a number of factors, including dehydration, sepsis, and heart failure. When blood flow to the kidneys is reduced, the kidneys are unable to filter waste products from the blood.
- Damage to the kidney cellscan occur due to a number of factors, including toxins, infections, and certain medications. When kidney cells are damaged, they are unable to filter waste products from the blood.
- Obstruction of the urinary tractcan occur due to a number of factors, including kidney stones, tumors, and blood clots. When the urinary tract is obstructed, urine is unable to flow out of the kidneys, which can lead to a buildup of waste products in the blood.
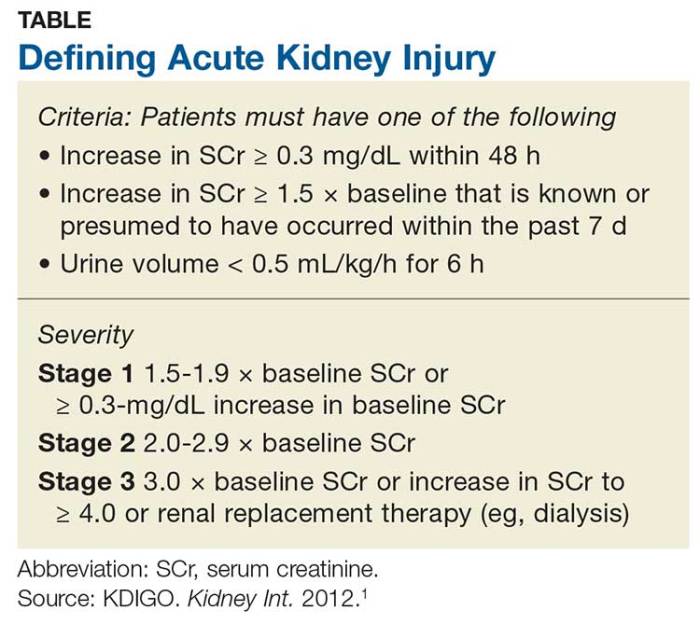
Stages of Acute Kidney Injury
AKI is typically classified into three stages: mild, moderate, and severe. The stage of AKI is determined by the level of creatinine in the blood. Creatinine is a waste product that is produced by the muscles. When the kidneys are unable to filter creatinine from the blood, the level of creatinine in the blood will increase.
- Mild AKIis defined as a creatinine level of 1.5 to 1.9 times the upper limit of normal.
- Moderate AKIis defined as a creatinine level of 2.0 to 2.9 times the upper limit of normal.
- Severe AKIis defined as a creatinine level of 3.0 times the upper limit of normal or greater.
Clinical Manifestations of Acute Kidney Injury
Acute kidney injury (AKI) is a sudden decline in kidney function. It can be caused by a variety of factors, including sepsis, dehydration, and certain medications. AKI can range in severity from mild to severe, and it can lead to a number of complications, including fluid overload, electrolyte imbalances, and death.
The clinical manifestations of AKI can vary depending on the severity of the injury. Mild AKI may cause few symptoms, while severe AKI can lead to a number of serious complications. The most common symptoms of AKI include:
- Decreased urine output
- Swelling in the hands, feet, and ankles
- Nausea and vomiting
- Fatigue
- Confusion
AKI can also lead to a number of laboratory and imaging findings. These findings can include:
- Increased blood creatinine levels
- Increased blood urea nitrogen levels
- Decreased glomerular filtration rate
- Ultrasound findings of enlarged kidneys
The complications of AKI can be serious and even life-threatening. These complications include:
- Fluid overload
- Electrolyte imbalances
- Acid-base imbalances
- Sepsis
- Death
AKI is a serious condition that requires prompt diagnosis and treatment. Early diagnosis and treatment can help to prevent the development of complications and improve the chances of a full recovery.
Nursing Management of Acute Kidney Injury
Nursing management of acute kidney injury (AKI) focuses on preventing further kidney damage, managing complications, and supporting the patient’s recovery. The goals of nursing care are to:
- Maintain fluid and electrolyte balance
- Prevent and treat complications
- Support the patient’s physical and emotional well-being
Nursing interventions for preventing and managing AKI include:
- Monitoring fluid intake and output
- Administering medications to maintain blood pressure and electrolyte balance
- Providing nutritional support
- Educating the patient and family about AKI
The nurse plays a vital role in patient education and support. The nurse should:
- Explain the nature of AKI and its treatment
- Provide information about the patient’s condition and prognosis
- Answer the patient’s and family’s questions
- Provide emotional support and counseling
Pharmacological Management of Acute Kidney Injury
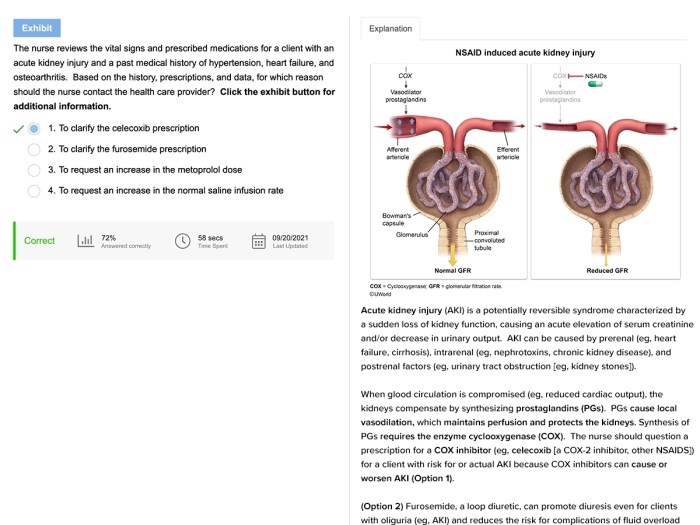
Pharmacological management of acute kidney injury (AKI) aims to address the underlying cause, prevent further deterioration, and support renal function. Various medications are employed based on the specific etiology and severity of AKI.
Medications Used in AKI, Nclex questions acute kidney injury
| Medication | Indication | Contraindications | Side Effects |
|---|---|---|---|
| Loop Diuretics (e.g., furosemide) | – Volume overload
|
– Severe hypotension
|
– Electrolyte imbalance
|
| Thiazide Diuretics (e.g., hydrochlorothiazide) | – Mild volume overload
|
– Severe renal impairment
|
– Electrolyte imbalance
|
| Mannitol | – Oliguria
|
– Severe heart failure
|
– Volume overload
|
| Sodium Bicarbonate | – Metabolic acidosis | – Alkalosis
|
– Fluid overload
|
| Acetaminophen | – Analgesia
|
– Liver disease
|
– Hepatotoxicity
|
| NSAIDs | – Pain relief
|
– Renal impairment
|
– Nephrotoxicity
|
| Aminoglycosides (e.g., gentamicin) | – Severe bacterial infections | – Renal impairment
|
– Nephrotoxicity
|
Role of the Nurse
Nurses play a crucial role in the pharmacological management of AKI. They are responsible for:
- Administering medications as prescribed.
- Monitoring patients for adverse effects and reporting any concerns to the healthcare provider.
- Educating patients and their families about the medications, their side effects, and the importance of adherence.
- Collaborating with other healthcare professionals to ensure a comprehensive approach to AKI management.
Fluid and Electrolyte Management in Acute Kidney Injury
Fluid and electrolyte management is a crucial aspect of managing acute kidney injury (AKI). It involves maintaining fluid and electrolyte balance, preventing fluid overload, and correcting electrolyte abnormalities.
The goal of fluid management is to maintain adequate hydration while avoiding fluid overload, which can exacerbate AKI. Fluids are typically administered intravenously, and the type and amount of fluid used depend on the patient’s individual needs.
Types of Fluids Used in AKI
- Isotonic fluids, such as normal saline (0.9% sodium chloride) and lactated Ringer’s solution, are used to maintain fluid balance and electrolyte levels.
- Hypotonic fluids, such as 0.45% sodium chloride, are used to correct hypernatremia.
- Hypertonic fluids, such as 3% sodium chloride, are used to correct hyponatremia.
Electrolyte Management in AKI
Electrolyte abnormalities are common in AKI and can lead to serious complications. The nurse plays a vital role in monitoring and managing electrolyte balance.
- Sodium: Hyponatremia (low sodium levels) is common in AKI and can cause seizures, coma, and death. Hypernatremia (high sodium levels) is less common but can also be life-threatening.
- Potassium: Hyperkalemia (high potassium levels) is a common and potentially fatal complication of AKI. Hypokalemia (low potassium levels) is less common but can also cause problems.
- Chloride: Chloride abnormalities are common in AKI and can lead to metabolic acidosis or alkalosis.
- Calcium: Hypocalcemia (low calcium levels) is common in AKI and can cause tetany, seizures, and arrhythmias.
- Magnesium: Hypomagnesemia (low magnesium levels) is common in AKI and can cause seizures, muscle cramps, and arrhythmias.
Nursing Management of Fluid and Electrolyte Balance
The nurse plays a crucial role in monitoring and managing fluid and electrolyte balance in patients with AKI. This includes:
- Assessing fluid status: The nurse assesses the patient’s fluid status by monitoring vital signs, daily weight, and urine output.
- Monitoring electrolytes: The nurse monitors the patient’s electrolytes through blood tests.
- Administering fluids and electrolytes: The nurse administers fluids and electrolytes as prescribed by the physician.
- Educating the patient: The nurse educates the patient about the importance of fluid and electrolyte balance and how to prevent complications.
Nutritional Management of Acute Kidney Injury
Nutritional management plays a crucial role in the recovery of patients with acute kidney injury (AKI). The primary goal is to provide adequate nutrition while avoiding further strain on the kidneys.
Nutritional Needs of Patients with AKI
- Increased protein requirements:To support tissue repair and prevent muscle wasting.
- Reduced fluid intake:As AKI affects the kidneys’ ability to excrete excess fluids.
- Electrolyte balance:Monitoring and adjusting electrolyte levels, such as potassium, sodium, and phosphorus, is essential.
- Adequate calories:To meet the increased energy demands of the body during AKI.
Types of Diets Used in Acute Kidney Injury
- Low-protein diet:Restricts protein intake to reduce the production of nitrogenous waste products.
- Fluid-restricted diet:Limits fluid intake to prevent fluid overload.
- Potassium-restricted diet:Restricts potassium intake to prevent hyperkalemia.
- Sodium-restricted diet:Restricts sodium intake to prevent fluid retention and hypertension.
Role of the Nurse in Providing Nutritional Support
- Assessment:Monitor nutritional status, fluid balance, and electrolyte levels.
- Education:Provide dietary counseling and education to patients and families.
- Collaboration:Work closely with the dietitian and healthcare team to develop individualized nutritional plans.
- Administration:Ensure proper administration of nutritional supplements and medications.
- Monitoring:Regularly monitor the patient’s response to nutritional interventions and adjust as needed.
Patient Education and Support in Acute Kidney Injury
Patient education and support play a crucial role in managing acute kidney injury (AKI). Empowering patients with knowledge and providing emotional support can improve outcomes and promote self-care.
Key Points for Patient Education
- Definition and causes of AKI
- Symptoms and signs of AKI
- Treatment options and potential complications
- Importance of medication adherence
- Dietary modifications and fluid restrictions
- Lifestyle changes to prevent future AKI
Methods of Patient Education
Patient education can be provided through:
- One-on-one sessions with healthcare professionals
- Written materials (e.g., pamphlets, brochures)
- Online resources (e.g., websites, apps)
- Support groups and peer education
Emotional Support for Patients and Families
Nurses play a vital role in providing emotional support to patients and their families coping with AKI. This involves:
- Listening to their concerns and providing reassurance
- Answering their questions and addressing misconceptions
- Providing information about support resources
- Empowering them to make informed decisions about their care
By providing comprehensive patient education and emotional support, nurses can help patients and their families navigate the challenges of AKI and promote positive outcomes.
Expert Answers
What are the common causes of acute kidney injury?
Pre-renal factors (e.g., hypovolemia, sepsis), intrinsic renal factors (e.g., glomerulonephritis, pyelonephritis), and post-renal factors (e.g., urinary tract obstruction).
What are the key nursing interventions for preventing acute kidney injury?
Maintaining adequate hydration, monitoring fluid balance, administering medications as prescribed, and avoiding nephrotoxic agents.
What are the potential complications of acute kidney injury?
Electrolyte imbalances, fluid overload, metabolic acidosis, and chronic kidney disease.